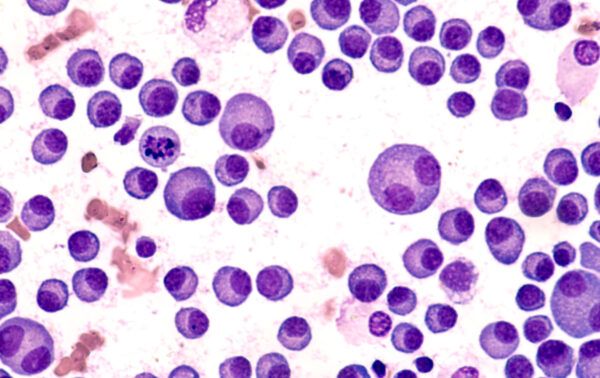
Multiple myeloma (MM) is a complex blood cancer affecting plasma cells. Patients can experience bone damage and fractures, kidney failure resulting from protein buildup, anemia and more frequent infections, among other symptoms. Given the disease’s serious impacts to quality and length of life, scientists are motivated to explore innovative therapies to help patients. Gene-edited cell therapies offer a tailored approach to combatting cancer while minimizing harm to healthy tissues. One possible candidate is CB-011, the gene-edited CAR-T cell therapy at the center of the CaMMouflage clinical trial (NCT05722418).1 In this review, we’ll delve into the scientific underpinnings of CB-011, examining the key elements that position it as a potential breakthrough in MM treatment.
At the heart of CB-011’s design lie targeted modifications to two pivotal genes: TRAC and B2M. The TRAC gene, responsible for encoding the T-cell receptor (TCR) alpha chain, plays a crucial role in the immune response against cancer cells. By editing the TRAC gene, scientists can suppress the expression of the cell’s endogenous TCR expression. Eyquem, et al. observed that targeting CAR transgene insertion to the TRAC locus mitigates T cell exhaustion, a key impediment to the efficacy of this category of cell therapies.2 Concurrently, modifications are made to the B2M gene, which encodes the beta-2 microglobulin protein. These alterations disrupt the expression of major histocompatibility complex (MHC) class I molecules on the cell surface. MHC class I molecules play a vital role in presenting antigens to the immune system, aiding in the identification and elimination of abnormal or infected cells. Interfering with MHC class I expression is aimed at evading surveillance by the host immune system.
In addition to these genetic adjustments, CB-011 is armed with a chimeric antigen receptor (CAR) designed specifically to target the B-cell maturation antigen (BCMA). BCMA is abundantly expressed on the surface of neoplastic plasma cells, making it an ideal target for a cell therapy meant for that diagnosis. With CAR-T cells engineered to recognize and bind to BCMA, CB-011 targets MM cells while minimizing damage to healthy tissues. This targeted approach not only enhances the therapeutic effectiveness of CB-011 but also reduces the risk of unintended effects commonly associated with conventional chemotherapy.
The journey of CB-011 from the laboratory to clinical application is thanks to extensive preclinical testing. Preliminary non-human studies resulted in reduction of tumor burden and longer lifespan, indicating effective anti-tumor activity. These promising findings have paved the way for the ongoing CaMMouflage phase 1 trial, which seeks to assess the safety, tolerability, and effectiveness of CB-011 in patients with relapsed/refractory MM.
Work is ongoing on many fronts towards innovative therapies for diagnoses with currently insufficient therapeutic options, such as is the case with refractory cancers. Much advancement has been achieved with edited T cells, including FDA-approved therapies, but research is underway with other cell types, such as Natural Killer cells. The outlook is promising for advancement in treatment options within the field of oncology.
Reference:
- Degagné, É., Donohoue, P. D., Roy, S., et al. (2024). High-specificity CRISPR-mediated genome engineering in anti-BCMA allogeneic CAR T cells suppresses allograft rejection in preclinical models. Cancer Immunology Research.
- Eyquem, J., et al. (2017). Targeting a CAR to the TRAC locus with CRISPR/Cas9 enhances tumour rejection. Nature, 543(7643), 113-117. doi.org/10.1038/nature21405
