The pace at which autologous CAR-T cells can be manufactured has been an obstacle for this very powerful technology from the start. Producing a cutting-edge cell therapy product in less than two weeks may sound fast, but those are two weeks patients may not have to spare when fighting against aggressive, refractory leukemias. Clinical trials involving CAR-T cell therapies may require that patients already have tried front-line treatment options in order to qualify. However, cancers may become more aggressive after surviving the initial treatment attempt, accumulating more mutations in the process. Time is of the essence for these patients, so researchers set out to accelerate CAR-T cell production while creating a safer product of more consistent quality.
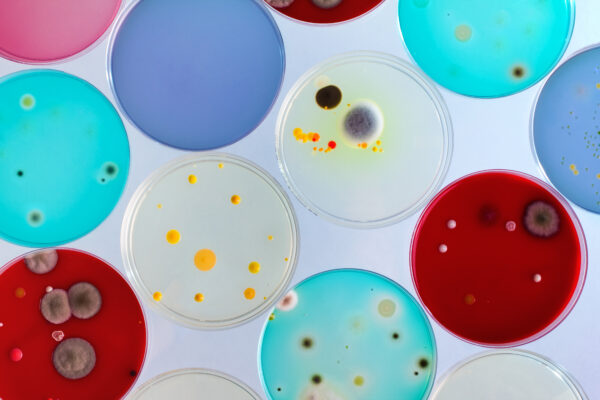
The original CAR-T manufacturing process in place at the National Cancer Institute took 10 days, without taking into account the time required to transport the sample or product between the facility and the patient. Firstly, peripheral blood is collected from the patient, from which Peripheral Blood Mononuclear Cells (PBMCs) are isolated via density gradient centrifugation. PBMCs consist of multiple immune cell types, including T cells. The original, manual manufacturing approach required a number of washing and centrifugation steps after separating the PBMC layer from the original blood product. Several steps involved opening the sample container, imparting a risk of microbial contamination. All of this was replaced with an automated method that would occur within an enclosed space, greatly reducing the contamination risk.[1] That risk mitigation removed the potential for lost time and samples, due to contamination.
The medium in which the isolated cells were to be grown was examined as well, with two goals: reducing the processing time to only six days, and eliminating the need for adding human serum. Human serum varies from one unit to the next in its ability to encourage cells to grow,[1] making process performance unpredictable. Several commercially available culture media were tested. Only one, when supplemented with T-cell serum replacement solution performed as well as the human serum-supplemented medium.[1]
As with the initial centrifugation steps, downstream transductions and stimulant additions were being performed in a manner vulnerable to microbial contaminants. The steps involved containers that had to be opened to the air like plates and flasks. A different process was tested in which the steps could be carried out inside bags coated with retronectin, which facilitates viral-mediated transduction.[2]
The many process changes were all tested in concert in five different production runs. CAR expression in the final product was measured using Fluorescence-Activated Cell Sorting (FACS). Interferon gamma (IFN-γ), a cytokine with many anti-tumor functions was measured using enzyme-linked immunosorbent assay (ELISA). When results could be compared between the two cell manufacturing methods, CAR-T cells manufactured using either process were “functionally and phenotypically indistinguishable.” [1]
The significance of improvements like these are far-reaching, most of all because enclosing and automating manufacturing processes can improve their scalability. CAR-T treatments will become more widely employed only insomuch as they can be mass-produced with short turnaround times. Improvements like these move us closer to that goal.
References
- Lu, T.L., Pugach, O., Somerville, R., et al. A Rapid Cell Expansion Process for Production of Engineered Autologous CAR-T Cell Therapies. Hum Gene Ther Methods. 2016 Dec;27(6):209-218. doi: 10.1089/hgtb.2016.120. Erratum in: Hum Gene Ther Methods. 2017 Apr;28(2):100. PMID: 27897048; PMCID: PMC6445175.
- Rajabzadeh, A., Hamidieh, A.A. & Rahbarizadeh, F. Spinoculation and retronectin highly enhance the gene transduction efficiency of Mucin-1-specific chimeric antigen receptor (CAR) in human primary T cells. BMC Mol and Cell Biol 22, 57 (2021). https://doi.org/1186/s12860-021-00397-z
