While T cells engineered with chimeric antigen receptors (CAR-T cells) have revolutionized the landscape of hematologic malignancy treatment, their efficacy against solid tumors remains limited. However, there is a promising alternative: Natural Killer T (NKT) cells. These innate-like T lymphocytes are unique contenders in the fight against cancer, offering unique immunotherapeutic advantages which differ from those of T cells and of Natural Killer (NK) cells.
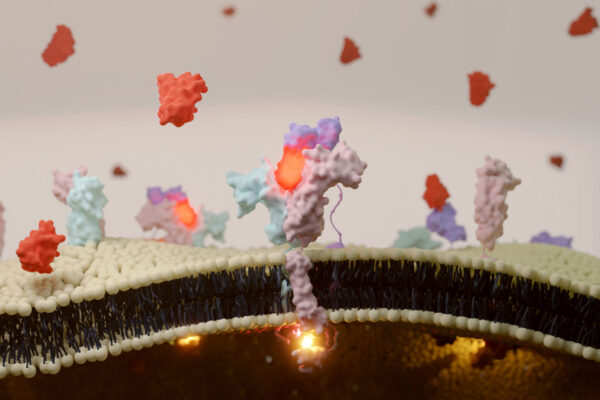
NKT cells stand out for their ability to recognize glycolipids presented the monomorphic major histocompatibility complex (MHC)-like molecule known as CD1d1. Unlike conventional T cells, NKT cells possess a distinctive T-cell receptor (TCR) that equips them to target a diverse array of tumor cells. This unique feature enables NKT cells to mount rapid responses to both microbial threats and malignant cells.
NKT cells can directly engage in cytotoxicity against cancerous cells, while also triggering additional immune responses through interaction with other immune cell populations. Notably, NKT cells play a pivotal role in shaping the tumor microenvironment by influencing the behavior of tumor-associated macrophages (TAMs), dendritic cells (DCs), and other immune cells. Through these interactions, NKT cells promote an environment conducive to tumor regression and immune-mediated destruction of cancer cells.
CAR-NKT cells represent a promising innovation, equipping them with chimeric antigen receptors targeting specific tumor antigens. Moreover, advancements in manufacturing techniques have paved the way for the production of allogeneic NKT cell therapies, offering a scalable and off-the-shelf solution for cancer treatment. Importantly, the safety profile of NKT cell therapies in early-stage trials appears promising, with minimal incidences of adverse events reported across various trials.
Efforts are underway to mitigate the risk of rejection by the recipient’s immune system. One approach involves human leukocyte antigen (HLA) knockdown, where techniques such as small hairpin RNA (shRNA) targeting B2M and CD74 are utilized to decrease the expression of HLA class I and II molecules, respectively, on NKT cells. By reducing the expression of these molecules, which serve as targets for immune recognition, the risk of rejection by the recipient’s T cells can be minimized.
Additionally, researchers are exploring immune evasion strategies such as modifying the expression of certain surface molecules on NKT cells. CD47 interacts with SIRPα on the surface of macrophages, helping NKT cells evade phagocytosis2. HLA-E is an inhibitory molecule that interacts with NK cells to suppress their cytotoxic activity against NKT cells. Furthermore, the production of multiple allogeneic NKT cell banks to promote partial HLA matching is being investigated as a means to reduce the likelihood of immune rejection.
Beyond cancer therapy, the unique properties of NKT cells hold promise for applications in treating other diseases, including autoimmune disorders and infectious diseases. Moreover, the success of NKT cell-based therapies may serve as a blueprint for harnessing the potential of other innate-like T cell subsets, opening new avenues for precision medicine and personalized immunotherapy. The possibility of transforming the lives of patients fighting cancer as well as other ailments seems to loom near, but only time will tell which of the many promising immunotherapeutic technologies on the horizon will make it to the clinic.
References
- Courtney, A. N., Tian, G., & Metelitsa, L. S. (2023). Natural killer T cells and other innate-like T lymphocytes as emerging platforms for allogeneic cancer cell therapy. Blood, 141(8).
- Jalil, A. R., Andrechak, J. C., & Discher, D. E. (2020). Macrophage checkpoint blockade: results from initial clinical trials, binding analyses, and CD47-SIRPα structure-function. Antibody therapeutics, 3(2), 80–94. doi.org/10.1093/abt/tbaa006
